What is Dental Sleep Medicine?
While CPAP continues to advance as a therapy for treating sleep breathing disorders, dental alternatives (snoring mouth guards and oral appliance therapy, or OAT) have recently been approved as first-line approaches to treating these same sleep disorders.
What is dental sleep medicine?
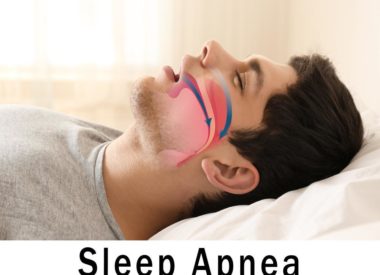
The American Academy of Dental Sleep Medicine (AADSM) defines it dental sleep medicine as “an area of dental practice that focuses on the use of oral appliance therapy to treat sleep-disordered breathing, including snoring and obstructive sleep apnea (OSA).”
In 2015, the AADSM and the American Academy of Sleep Medicine (AASM) collaborated on a position paper to set new standards for the use of dental services, both as an alternative and as an initial treatment for either sleep disorder.
The history of dental sleep medicine
To some extent, dentists and physicians have always worked together to help patients with their sleep breathing problems. CPAP has long been used as the first line of therapy for treating these problems, but recent studies now show that patients who use OAT can experience equally successful treatment and demonstrate high compliance rates.
Certain sleep disorders ( snoring, upper airway resistance syndrome, bruxism, and OSA) have been of chief concern to dentists. They are trained to quickly identify risk factors for them at chair side and know to make necessary referrals to sleep specialists.
Snoring has long been considered a key risk factor for developing OSA. It was dentists, three decades ago, who pioneered the snoring mouthpiece as a therapeutic category to curb the problem. As more people with severe snoring used them, it became apparent that, in some cases, their usage also meant successful treatment for cases of mild to moderate OSA.
Dental researchers looked to more complex approaches for building these mouth guards. The approaches allowed for some adjustment of their moving parts in order to control the two parts of the upper airway most inclined to collapse and cause apneas: the tongue (by sliding into the back of the throat), and the lower jaw (by recessing into the back of throat).
By building mouthpieces that prevented obstructions to breathing, dentists have been able to develop devices which not only eliminate snoring, but which can reduce the likelihood of apneas. When users gain more room to breathe in the back of the airway, they also gain improvements in the firmness of the tissues of the upper airway, which often collapse because they are flabby or overlarge.
How can dentists help with sleep disorders?
Primary care physicians may not always recognize the relationship between certain “quiet” signs of untreated sleep apnea. These include:
- a thick neck (added weight can cause obstructed breathing when the patient reclines)
- insomnia complaints (which could be due to unidentified and untreated OSA)
- an overlarge tongue or uvula(as potential obstructions)
- morning headache (to signal hypoxia in the final hours of sleep, especially during REM )
- a “soft” or receding chin (as a potential obstruction)
- narrow dental arches (which can lead to a crowded mouth)
- an unexplained rise in blood pressure (which could be caused by unidentified and untreated OSA)
- narrow nasal or sinus passages (which lead to airway resistance and allergy-related problems like postnasal drip and congestion)
- depressive symptoms (as a signal of sleep deprivation caused by unidentified and untreated OSA)
- low energy (because of sleep fragmentation potentially caused by a sleep breathing disorder)
- daytime sleepiness (because of sleep fragmentation caused by a sleep breathing disorder)
Dentists also encounter a lot of patients who show characteristic behaviors that point to potential sleep breathing disorders. A few examples are listed below:
-
They fall asleep in the chair
-
They can’t “open wide” during exams
-
Their teeth show patterns of grinding at night
-
They complain of jaw pain in the morning
-
They struggle to breathe in the dentist’s chair when it is reclined at a certain angle
These are potential “red flags” that dentists can use to refer patients on to sleep specialists for further assessment.
Dentists can easily screen for OSA. Since they often see some patients more frequently than the patients’ sleep doctors do, they have the added benefit of gathering objective data from exams and x-rays to show changes in physiology that could support the diagnosis of a sleep breathing disorder.
What are the dental-based treatments for sleep apnea?
There are two main ways that dentists can provide therapeutic treatments for sleep breathing disorders:
Dental appliances (also called oral devices or mandibular advancement devices [MAD]) splint open the upper airway during sleep to prevent obstructions. They are worn like mouth guards so they are custom built to fit the patient’s bite. These devices reposition the lower jar and tongue forward, which alters the upper airway structure in such a way as to allow for unobstructed breathing.
Snoring mouthpieces (also called snore guards ) are often less complex in design than dental appliances. The goal of this therapy is much the same: to help advance the lower jaw to reduce vibrations in the airway caused by floppy, extraneous tissues in the throat and mouth which can create the friction that leads to primary snoring.
Dentists with board-certified dental sleep medicine are skilled in building and fitting most of these devices, and the sleep clinic is the proper place to test and titrate them. In a concerted effort between both specialties, many patients can overcome their sleep breathing problems knowing they have support from two medical fields.
Why does dental sleep medicine matter?
CPAP has been a boon for thousands of patients, who eagerly attest to its life-altering treatment.
However, some patients, through no fault of their own, simply cannot abide CPAP. People who have allergies, preexisting claustrophobia, or a deviated septum, for instance, may not succeed at using this therapy (though some do).
For others, CPAP therapy has uncomfortable side effects that, even with the most tenacious efforts, some patients simply can’t tolerate.
OAT offers a viable solution that may help them comply with their therapy and achieve the same outcomes as those who use CPAP. It’s also been shown that, even when an oral device does not measure as high in effectiveness as a CPAP machine does when treating OSA, the chances that a patient will use the oral device are often much higher than they are for using a CPAP machine.
Dental sleep medicine recognizes the needs of patients who cannot use CPAP and has worked with sleep specialists to build a new cooperative model to partner board-certified dentists trained in sleep medicine with sleep specialists to prioritize patient-centered care.
Dentists: Part of the new sleep medicine team
Dentists are not able to diagnose medical illnesses, but that does not mean they cannot contribute to a larger team effort. They can still refer patients with potential sleep disorders to sleep specialists when their complaints, key symptoms, and other physiological evidence all add up to a likely diagnosis.
The demand for dentists trained and board-certified in dental sleep medicine has never been higher. Many are going back to school to take part in clinical training or mini-residencies in dental sleep medicine, and post-graduate institutes now provide continuing dental education. Some dentists have even changed their practices to a “dental sleep medicine only” specialty to meet the need.
Dentists have long worked with physicians to screen for other health concerns like oral cancer and high blood pressure. It’s a natural progression for them to join the sleep medicine team, since they are already primed to identify and treat sleep breathing disorders.
American Academy of Dental Sleep Medicine
American Academy of Sleep Medicine