The high price of untreated sleep apnea
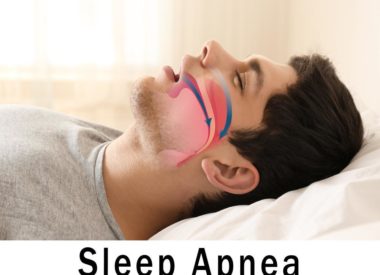
After insomnia, sleep apnea is the most common sleep disorder in the US, affecting nearly 20 million Americans.
As much as10 percent of the entire US adult population suffers from obstructive sleep apnea (OSA), the most common form of sleep apnea.
Anywhere between 40 and 80 percent of people with OSA may not even know they have it, or if they do have it, are not treating it.
The risks of living with untreated sleep apnea far outweigh the efforts needed to invest in continuous positive airway pressure (CPAP) therapy to treat it.
Without proactive compliance to CPAP therapy, those with sleep apnea are setting themselves up for a lifetime of chronic health problems as well as a higher likelihood of suffering from injuries.
In addition, the higher healthcare expenses that come with untreated OSA, and the reduction in quality of life that is also part of the cost of not treating it, make one thing clear:you can’t ignore a sleep apnea problem without paying a price.
What are the risks of ignoring sleep apnea?
Chronic disease
The American Academy of Sleep Medicine (AASM) reports that people with moderate to severe OSA are “four times more likely to die when [sleep apnea] is left untreated in the long term.” They list these negative long-term health consequences for those who think they can just ignore sleep apnea:
-
High blood pressure and stroke
-
Heart disease (coronary artery disease, congestive heart failure, cardiac arrhythmia)
-
Pre-diabetes and diabetes
-
Depression
The president of the AASM, Dr. Safwan Badr, makes itclear: “Obstructive sleep apnea is a chronic disease that can be destructive to your health.”
Other research shows even more problems which are also independently linked to untreated sleep apnea:
-
Cancer patients with untreated OSA are four times more likely to die when compared to those without OSA or who treat their OSA proactively, says a study in the Journal of Clinical Sleep Medicine .
-
A link exists between undiagnosed or untreated OSA and increased adverse outcomes for surgical patients, as shown by research conducted by Dr. Vishesh Kapur at the University of Washington. Their research showed that those with untreated OSA are more likely to experience respiratory failure while under general anesthesia.
-
Without active treatment of sleep apnea, someone with OSA is more likely to suffer from chronic kidney disease, according to research published in Thorax in 2015 that observed outcomes for more than 3 million veterans with OSA.
Injury risks
Untreated OSA leads to sleep deprivation ; this is because sleep is interrupted continuously by lengthy pauses in breathing that can lead to ongoing issues with hypoxia (low blood oxygen). This disrupted sleep prevents you from getting the healing, restorative rest your body and brain need to function while awake.
Accidents and injuries are a public safety problem that relates directly to sleep deprivation, according to the Centers for Disease Control and Prevention.
For instance, someone with untreated OSA (or who is avoiding or ignoring their prescribed sleep apnea treatment)is three times more likely to have a workplace accident or sustain an injury while on the job. For motor vehicle accidents, undiagnosed OSA can lead to a 20 percent increase in the risk for sleep-related traffic accidents.
Sleep deprivation causes, among other things, impaired vigilance, a reduction in the ability to adequately perform daily tasks while on the job, and a greater chance you’ll make poor decisions and egregious errors during your work day.
The economic burden of untreated OSA
In 2004, one study of automobile accidents linked to OSA (estimated at 800,000 annually) showed that nearly 1500 resulted in fatalities, with $16 billion in costs attributed to those accidents.
More recently, the AASM commissioned several white papers to report on the state of OSA as it pertains to public health expenditures. They discovered that under diagnosing and failing to treat OSA has become an expensive drain on the entire healthcare system.
Immediate past president of the AASM, Dr. Nathaniel Watson, published an eye-opening editorial this summer on the results of the findings in these white papers: ” Health Care Savings: The Economic Value of Diagnostic and Therapeutic Care for Obstructive Sleep Apnea.”
In the aforementioned UW study, Dr. Kapur and his team also found that the mean annual healthcare costs for someone with untreated OSA were nearly twice those of someone without OSA.
Who suffers the economic burden?
People with OSA are 10 times more likely to file for workplace disability, which drives up employment costs and reduces overall productivity.
They also spend more time and money engaged in healthcare concerns, as expressed in the results of multiple research studies that measure healthcare costs among those in this patient population.
Other entities that feel the pinch include insurance companies, Medicare, and healthcare professionals, which leads to increases in rates and reimbursements as well as more strict protocols to weed out system abusers and noncompliant patients.
Lost: Quality of Life
Forget about the practical benefits of treating OSA. What about simply feeling better and having the energy and focus to live a fully realized life?
The sleep deprivation that results from untreated OSA makes it difficult to get out of bed in the morning, causes problems with daytime sleepiness, and leaves sufferers with hypersensitivity to pain, cognitive fogginess, and irritability.
Not surprisingly, outcomes of these unpleasant and adverse effects of untreated sleep apnea include job dissatisfaction, burnout, and relationship stress.
What are you waiting for? If you think you have sleep apnea, investing in a sleep study, confirming a diagnosis, and applying CPAP therapy could be the best investment you ever make in your health.
If you’ve already been diagnosed, please practice compliance with your therapies. If that means you need to come back to treatment after a significant time away, so be it. A sleep specialist can quickly and easily help you get back on track… but only if you ask for help.
In the meantime, check out our free downloadable e-book below for information about starting PAP, if you are planning to make a return or are curious about this highly effective OSA treatment.
Sources:
American Academy of Sleep Medicine
Centers for Disease Control
Journal of Clinical Sleep Medicine
National Sleep Foundation
Thorax